Dietary Do’s and Don’ts for Anaemia: Foods, Meal Tips & Smart Testing
Anaemia is one of the most common nutritional problems in India and worldwide. It can make you feel tired, weak, breathless, and less productive in your daily life. The good news: in many cases, anaemia can be prevented and managed effectively with the right diet, lifestyle changes, and timely lab tests.
This comprehensive guide explains:
- What anaemia is and why it happens
- Types of anaemia and their common causes
- Dietary do’s and don’ts for different types of anaemia
- Best food combinations to improve iron absorption
- Key lab tests and health packages from Seralis Lab you should consider
- FAQs and scientifically backed references
What Is Anaemia?
Anaemia is a condition in which the number of red blood cells (RBCs) or the haemoglobin (Hb) level in the blood is lower than normal. Haemoglobin is an iron-rich protein in RBCs that carries oxygen to all parts of your body. When you are anaemic, your tissues and organs receive less oxygen, leading to fatigue and poor performance.
Common Symptoms of Anaemia
- Persistent tiredness and low energy
- Pale skin, lips, and nail beds
- Shortness of breath on mild exertion
- Dizziness or lightheadedness
- Headaches
- Fast or irregular heartbeat
- Cold hands and feet
- Brittle nails or hair loss
Symptoms can be mild initially and often go unnoticed. That is why regular blood testing is important if you are at risk.
Major Types of Anaemia & Nutritional Links
Anaemia is not a single disease. There are several types, many of which are strongly linked to diet and nutrient deficiencies.
1. Iron Deficiency Anaemia (IDA)
This is the most common type. It occurs when your body does not have enough iron to make haemoglobin.
Common causes:
- Inadequate intake of iron-rich foods (especially in vegetarians/vegans)
- Heavy menstrual bleeding
- Pregnancy (increased iron demand)
- Chronic blood loss (e.g., piles, ulcers, gastrointestinal bleeding)
- Poor absorption of iron due to gut issues (e.g., celiac disease)
2. Vitamin B12 Deficiency Anaemia
Also called megaloblastic or pernicious anaemia (if due to autoimmune causes). Vitamin B12 is essential for red blood cell formation and nerve function.
Common causes:
- Low intake of animal foods (strict vegans, elderly)
- Poor absorption (gastric surgery, chronic gastritis, intrinsic factor deficiency)
- Certain medications (e.g., prolonged use of metformin, proton pump inhibitors)
3. Folate (Vitamin B9) Deficiency Anaemia
Folate is another B vitamin needed for RBC production and cell division.
Common causes:
- Diet low in green leafy vegetables, legumes, and fruits
- Increased requirement (pregnancy, growth, haemolytic anaemia)
- Alcohol excess, certain medications (e.g., methotrexate, phenytoin)
4. Anaemia of Chronic Disease
Also called anaemia of inflammation. It occurs in chronic infections, autoimmune diseases, kidney disease, and cancers. Iron stores may be normal or high, but the body is unable to use iron properly.
Note: Dietary changes alone may not be enough if you have anaemia of chronic disease or inherited disorders (like thalassemia, sickle cell disease). You must follow your doctor’s treatment plan.
Nutrition Goals in Anaemia
The dietary strategy depends on the type of deficiency, but in general you want to:
- Increase intake of iron-rich foods (especially if iron deficiency anaemia)
- Ensure adequate vitamin C to enhance iron absorption
- Include vitamin B12 and folate-rich foods
- Avoid or limit substances that block iron absorption at key meals
- Maintain overall balanced nutrition with enough protein and calories
Before heavily changing your diet or starting supplements, confirm your deficiency type with appropriate lab tests.
Essential Lab Tests for Anaemia Evaluation
Proper diagnosis guides the right diet and treatment. Consider these key tests:
1. Complete Blood Count (CBC / Haemogram)
A CBC gives haemoglobin, RBC count, haematocrit, MCV, MCH, MCHC, and more—crucial for identifying and classifying anaemia.
Recommended test: Haemogram (CBC)
2. Iron Studies
- Serum iron
- Total iron-binding capacity (TIBC)
- Transferrin saturation
- Serum ferritin (reflects iron stores)
Recommended package: Anaemia Profile – Basic (includes CBC, iron studies, and ferritin – ideal for suspected iron deficiency)
3. Vitamin B12 and Folate Levels
To detect megaloblastic anaemia due to deficiency of B12 or folate.
Recommended package: Vitamin Profile – B12, D & Folate (useful if you suspect multiple vitamin deficiencies)
4. Comprehensive Anaemia Workup
If you have persistent anaemia or your doctor wants a detailed view, choose a more extensive package that combines CBC, iron parameters, B12, folate, and inflammatory markers.
Recommended package: Anaemia Profile – Advanced
5. General Health Check Packages (If You Have Multiple Risk Factors)
Many people with anaemia also have nutritional issues, thyroid imbalance, or chronic diseases. In such cases, choose a wider health package.
These packages help identify associated issues like thyroid disorders, kidney problems, inflammation or infections which can worsen anaemia.
Dietary Do’s for Anaemia
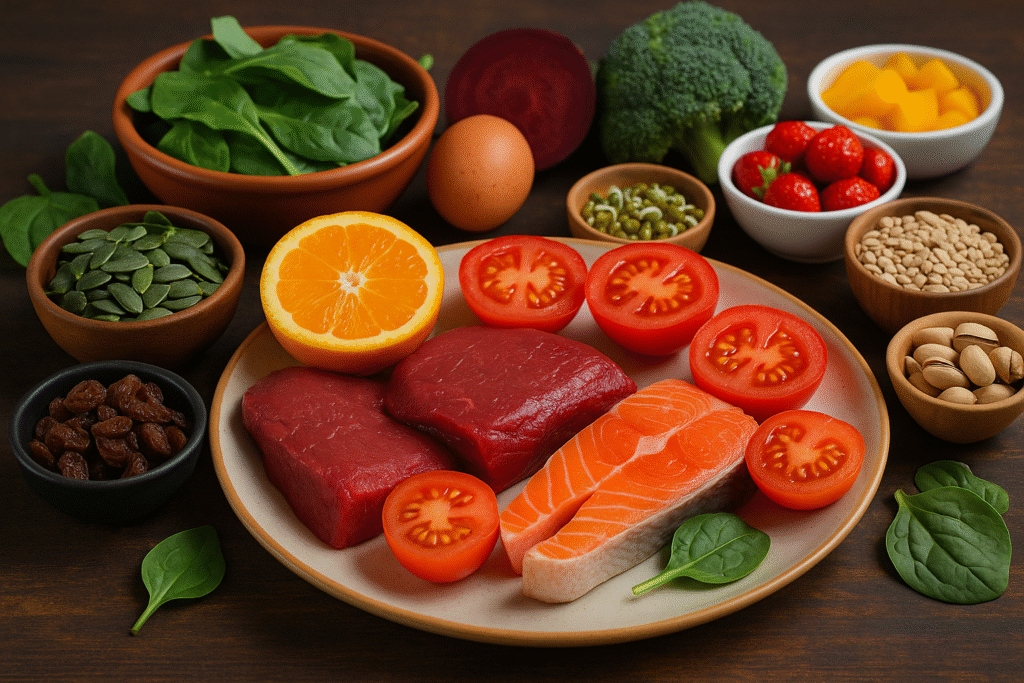
1. Include Iron-Rich Foods Daily
Haem Iron (Better Absorbed – From Animal Sources)
- Lean red meat (in moderation)
- Chicken, turkey
- Fish and seafood (sardines, mackerel, tuna, shellfish)
- Eggs (particularly yolk)
Non-Haem Iron (Plant Sources)
These are vital in vegetarian diets but are less easily absorbed. Combine with vitamin C for better absorption.
- Green leafy vegetables – spinach, methi (fenugreek leaves), amaranth, mustard leaves, bathua
- Pulses and legumes – rajma (kidney beans), chana, masoor dal, moong, soybeans
- Whole grains – bajra (pearl millet), ragi, whole wheat, quinoa, oats
- Nuts and seeds – pumpkin seeds, sesame seeds (til), flaxseeds, cashews, almonds
- Jaggery (gur) – use moderately; it contains some iron but is still a sugar
- Dried fruits – raisins, dates, prunes, apricots
2. Pair Iron with Vitamin C
Vitamin C significantly boosts absorption of non-haem iron. Add a vitamin C source to your major meals.
Vitamin C-rich foods:
- Citrus fruits – oranges, mosambi, lemon
- Guava, amla (Indian gooseberry)
- Kiwi, strawberries, papaya
- Tomatoes, capsicum, broccoli
- Fresh lemon juice on dal, sabzi, salad
Practical tip: Squeeze lemon on your dal, chole, or palak sabzi; have a small bowl of fruit (like orange or guava) along with iron-rich meals.
3. Make Smart Use of Cooking Methods
- Use cast iron pans for cooking; they can slightly increase iron content in food.
- Avoid overcooking vegetables – light steaming or sautéing helps preserve nutrients.
- Soak, sprout, or ferment grains and pulses to reduce phytates and improve mineral absorption.
4. Eat Enough Protein
Protein is necessary for haemoglobin production and repair of tissues.
- Animal sources: eggs, lean meats, fish, curd, paneer
- Plant sources: dals, chana, rajma, tofu, soy products, nuts, seeds
5. Focus on Vitamin B12-Rich Foods (If Non-Veg or Lacto-Ovo Veg)
- Eggs
- Fish and seafood (salmon, sardines)
- Meat (in moderation)
- Milk, curd, cheese (for vegetarians)
- Fortified cereals or plant milks (check labels for B12)
6. Increase Folate Intake
- Green leafy vegetables (spinach, methi, sarson)
- Asparagus, broccoli, Brussels sprouts
- Pulses – masoor dal, moong dal, chana dal
- Citrus fruits, avocado, beetroot
7. Keep Yourself Hydrated
Mild dehydration can worsen fatigue. Aim for 1.5–2.5 litres of fluids per day (water, herbal teas, soups, lemon water), depending on your climate, activity, and doctor’s advice.
Dietary Don’ts for Anaemia
1. Avoid Tea & Coffee with Main Meals
Tea and coffee contain tannins and polyphenols which significantly reduce iron absorption, especially from plant foods.
- Do not drink tea/coffee 1 hour before or after iron-rich meals.
- If you must have them, keep them away from breakfast and lunch that contain dal, greens, or fortified cereals.
2. Limit High-Calcium Foods at Iron-Rich Meals
Calcium competes with iron for absorption. High doses of calcium (e.g., supplements) near iron-rich meals can reduce iron uptake.
- Avoid taking calcium supplements together with iron tablets.
- Do not combine large amounts of milk products (like paneer, curd) with your main iron supplement dose – spread them apart by a couple of hours.
3. Watch Out for Phytates and Oxalates
These compounds in whole grains, some legumes, and certain vegetables can reduce iron absorption. This does not mean you should avoid them entirely, but use preparation techniques that reduce their effect.
- Soak and sprout legumes and grains.
- Ferment batters (idli, dosa).
- Pair with vitamin C sources to offset the inhibition.
4. Limit Highly Processed & Junk Foods
- Aerated drinks, chips, packaged snacks, instant noodles
- Excess sweets and refined flour products
These are calorie-dense but nutrient-poor and can worsen deficiencies.
5. Avoid Self-Medicating with Iron or B12 Injections
Unsuitable supplementation can cause side effects (e.g., constipation, toxicity or masking other deficiencies). Always test first and consult a doctor.
Use diagnostic tests such as the Anaemia Profile – Basic or Vitamin Profile – B12, D & Folate to identify what you truly need.
Suggested Sample Meal Ideas for Anaemia
Breakfast Options
- Vegetable upma with peas and carrots + lemon water + a slice of papaya
- Besan chilla with spinach + mint-coriander chutney + orange
- Oats porridge with nuts and seeds + guava
Mid-Morning Snack
- Handful of roasted chana and raisins
- Fruit salad with amla or oranges
Lunch Ideas
- Palak dal + brown rice/roti + salad with lemon dressing
- Rajma chawal + mixed vegetable sabzi + buttermilk (away from iron tablets)
- Chole with bhatura or phulka + kachumber salad + nimbu pani
Evening Snack
- Sprouted moong chaat with onions, tomatoes, coriander, and lemon
- Nuts and seeds trail mix (pumpkin seeds, almonds, walnuts)
Dinner Ideas
- Fish curry with rice + stir-fried vegetables
- Egg bhurji + multigrain roti + methi sabzi
- Tofu or paneer bhurji + dal + salad
Customise portions and recipes according to your calorie requirements, cultural preferences, and medical advice.
Special Considerations for High-Risk Groups
1. Women of Reproductive Age
- Increased risk due to monthly blood loss.
- Ensure iron-rich foods throughout the month, not just during periods.
- Annual screening with CBC and, if needed, Anaemia Profile – Basic is advisable.
2. Pregnant and Lactating Women
- Higher requirement for iron, folate, and B12.
- Your gynaecologist will usually prescribe supplements, but diet must also support increased needs.
- Regular monitoring with Anaemia Profile – Advanced or appropriate pregnancy panels is recommended.
3. Children and Adolescents
- Rapid growth demands more iron and folate.
- Avoid filling children up with junk food and sugary drinks.
- If your child is pale, fatigued, or has poor attention, discuss testing a CBC with your paediatrician.
4. Elderly
- May have reduced stomach acid, affecting B12 absorption.
- Check Vitamin B12 levels periodically, especially in vegetarians.
- Comprehensive packages like Wellness Package – Comprehensive help track multiple age-related conditions.
Lifestyle Tips Along with Diet
- Get adequate sleep: 7–9 hours of quality sleep aids recovery.
- Moderate exercise: Light activities like walking, yoga, or stretching can improve circulation and energy levels. Avoid over-exertion if your Hb is very low.
- Avoid smoking and excess alcohol: These can damage RBCs and interfere with nutrient absorption.
- Manage chronic diseases: Conditions like kidney disease, thyroid disorders, and autoimmune illnesses contribute to anaemia—regular check-ups are essential.
When to See a Doctor Immediately
Seek medical help urgently if you notice:
- Severe fatigue interfering with daily tasks
- Chest pain, extreme breathlessness, or palpitations
- Fainting spells
- Very pale or yellowish skin
- Black, tarry stools or visible blood in stools or urine
- Sudden worsening of symptoms
Your doctor may advise urgent tests like CBC, Advanced Anaemia Profile, or others based on your condition.
FAQs About Diet and Anaemia
1. Can anaemia be cured by diet alone?
Mild iron deficiency or early vitamin deficiencies can often be corrected with a proper diet and oral supplements. However, moderate to severe anaemia, anaemia due to chronic disease, or inherited conditions usually require medical treatment in addition to diet. Always confirm the cause through tests like the Anaemia Profile – Basic or Advanced Anaemia Profile.
2. How long does it take to improve haemoglobin with diet?
It typically takes 4–8 weeks of consistent dietary changes and/or supplements to see a noticeable increase in haemoglobin, and up to 3–6 months to fully replenish iron stores, depending on severity and cause. Repeat CBC and iron studies as advised by your doctor.
3. I am vegetarian. Can I still manage my anaemia without eating meat?
Yes, but you must be more deliberate about your food choices. Focus on iron-rich plant foods (greens, pulses, seeds, jaggery, dried fruits) and always pair them with vitamin C sources (lemon, amla, citrus fruits). You may also need supplements if your levels are low, especially for Vitamin B12, which is mostly found in animal foods.
4. Are jaggery and dates enough to treat anaemia?
Jaggery and dates contain some iron and can support your overall intake, but they alone are not enough to treat established anaemia. Over-reliance can also increase your sugar intake. Use them as part of a balanced diet, and follow your doctor’s advice based on tests like the Anaemia Profile – Basic.
5. Should I avoid milk completely if I have iron deficiency anaemia?
No, you do not need to completely avoid milk or dairy. Just avoid taking them together with your iron-rich meals or iron supplements. Keep a gap of 1–2 hours. Dairy products are still useful sources of protein and calcium for bone health.
6. How often should I test my haemoglobin and iron levels?
- If you are at high risk (women with heavy periods, pregnancy, chronic illness), at least once a year or as advised by your doctor.
- During active treatment of anaemia, you might need a CBC and iron profile every 6–12 weeks to track improvement.
7. Is it safe to take over-the-counter iron tablets without testing?
Not advisable. Excess iron can accumulate and damage organs, especially if your anaemia is not due to iron deficiency (for example, in thalassemia or anaemia of chronic disease). Always get tested first using a reliable anaemia panel and take supplements only under medical supervision.
Key Takeaways
- Anaemia is common but often preventable and treatable, especially when addressed early.
- Diet plays a central role: include iron, vitamin C, B12, and folate in your daily meals.
- Avoid tea/coffee around meals and be mindful of factors that block iron absorption.
- Do not rely solely on “home remedies”; confirm your deficiency with appropriate tests.
- Use targeted lab packages from Seralis Lab such as:
- Always discuss your reports and diet with your doctor or a qualified nutritionist.
References
- World Health Organization. Anaemia – Fact sheet.
- World Health Organization. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Geneva: WHO; 2020.
- National Institutes of Health, Office of Dietary Supplements. Iron – Fact Sheet for Consumers.
- National Institutes of Health, Office of Dietary Supplements. Vitamin B12 – Fact Sheet for Consumers.
- National Institutes of Health, Office of Dietary Supplements. Folate – Fact Sheet for Consumers.
- Zimmermann MB, Hurrell RF. Nutritional iron deficiency. Lancet. 2007;370(9586):511–520.
- Iqbal S, Ahmed I, et al. Prevalence of iron deficiency anemia and its dietary pattern among women of reproductive age. J Family Med Prim Care. 2022;11(3):946–952.
- Allen LH. Causes of vitamin B12 and folate deficiency. J Nutr. 2008;138(3):438–442.
This article is for educational purposes and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your doctor for personalised recommendations.