Side Effects of Using Breast Pumps: What Every Mother Needs to Know
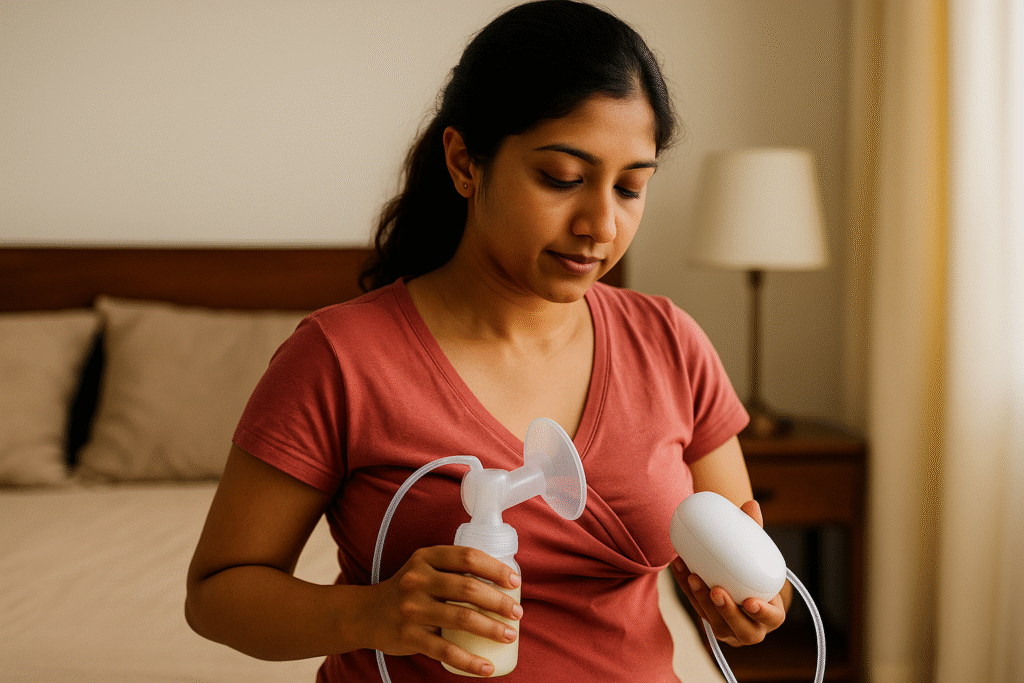
Breast pumps can be a lifesaver for new mothers — helping you store milk, return to work, or manage feeding challenges. But like any medical device, using a breast pump incorrectly or too frequently can lead to discomfort and even health issues.
This article explains the common side effects of breast pump use, how to prevent them, and when to seek medical help. We also highlight relevant lab tests and health packages from Seralis Lab that can support your postnatal and breastfeeding health.
What Is a Breast Pump and Why Is It Used?
A breast pump is a device that helps you extract breast milk either manually (hand pump) or using electric or battery-powered suction. Mothers may use breast pumps to:
- Store milk for later feeds
- Maintain supply when away from the baby
- Relieve engorgement
- Support babies who cannot latch properly
- Donate breast milk
While pumping is generally considered safe, improper use, poor hygiene, or incorrect sizing can cause complications.
Common Side Effects of Using Breast Pumps
1. Nipple Pain and Soreness
Mild nipple discomfort is common when you first start pumping. However, persistent or severe pain is a sign that something is wrong.
Causes
- Incorrect flange size (too small or too large)
- Excessive suction settings
- Improper positioning of the nipple in the flange
- Prolonged pumping sessions without breaks
How to manage and prevent
- Use the correct flange size as per pump manufacturer’s guide.
- Start with the lowest suction setting and increase gradually until comfortable.
- Apply lanolin-based nipple cream after pumping (if recommended by your doctor).
- Allow nipples to air-dry after each session.
If pain persists or nipples develop cracks or bleeding, consult a lactation consultant or gynecologist.
2. Nipple Damage, Cracks, and Blisters
Repeated friction and strong suction can lead to nipple trauma, including:
- Cracks and fissures
- Blisters or blood blisters
- Scabbing and bleeding
Why this is serious
Damaged nipples are more prone to bacterial and fungal infections. They can also make direct breastfeeding extremely painful, affecting your milk supply and bonding.
What you can do
- Check flange fit and reduce suction intensity.
- Limit pumping session length (typically 15–20 minutes per session, unless advised otherwise).
- Use warm compresses before pumping to soften the areola and improve milk flow.
- Seek medical help if you notice pus, worsening pain, or fever.
3. Breast Engorgement and Blocked Ducts
While breast pumps often help relieve engorgement, incorrect use or irregular pumping patterns can sometimes worsen engorgement or cause blocked milk ducts.
Symptoms of engorgement
- Breasts feel overly full, heavy, and painful
- Skin may appear tight, shiny, and warm
- Difficulty latching for the baby
Symptoms of blocked ducts
- Localised tender lump in the breast
- Discomfort that worsens before a pumping or feeding session
- Relief after milk removal
How pumping contributes
- Over-pumping can signal your body to produce more milk than the baby needs, leading to engorgement.
- Inadequate emptying of the breast during pumping can cause milk stasis and blocked ducts.
Prevention and relief
- Follow a pumping schedule that matches your baby’s feeding needs.
- Massage your breasts gently while pumping to encourage drainage.
- Use warm compresses before pumping and cold compresses afterward for pain relief.
- Alternate between breasts and avoid skipping pumping sessions suddenly.
If blocked ducts persist for more than 48 hours or are accompanied by fever or flu-like symptoms, you may be developing mastitis and need medical attention.
4. Mastitis and Breast Infections
Mastitis is inflammation of the breast tissue, often associated with infection. Using a breast pump with poor hygiene or not emptying the breast properly can increase the risk.
Signs and symptoms
- Red, swollen, painful area on the breast
- Fever and chills
- Body aches and fatigue
- Burning sensation while feeding or pumping
How breast pumps can contribute
- Inadequate breast emptying → milk stasis → inflammation
- Dirty pump parts → bacterial contamination
- Damaged or cracked nipples → entry point for infection
When to get tested
If you have fever, severe pain, or suspect infection, your doctor may recommend:
- Complete Blood Count (CBC) to check signs of infection and inflammation.
- In some cases, breast milk culture to identify the bacteria causing the infection (ordered by your doctor).
You can explore relevant health checks such as:
- Postnatal / Women’s Health Profiles (for overall postpartum health, including infection markers).
Mastitis often requires antibiotics, so do not delay consulting a doctor if you notice these symptoms.
5. Decreased Milk Supply Due to Incorrect Pumping
While pumping is often used to maintain or increase milk supply, using it incorrectly can sometimes signal the body to produce less milk.
Possible reasons
- Infrequent pumping sessions
- Short sessions that do not fully empty the breast
- Poorly fitting flange affecting milk removal efficiency
- Stress, fatigue, dehydration, or hormonal issues
Tips to support milk supply
- Ensure regular and complete drainage of the breasts (by baby, pump, or both).
- Maintain good hydration and nutrition.
- Get as much rest as possible and seek family support.
- Consult a lactation consultant if supply seems to be dropping.
If low milk supply is persistent, your doctor may also check for underlying hormonal or metabolic conditions (like thyroid issues or anemia). In such cases, consider relevant tests like:
- Thyroid Function Tests (TSH, T3, T4)
- Anemia Profile / Iron Studies / CBC
6. Breast Tissue Trauma and Bruising
Using a high suction setting or pressing the flange too hard on the breast can cause:
- Bruising around the areola
- Swelling and tenderness
- Temporary changes in breast shape
How to avoid this
- Always start with low suction and increase only to a comfortable level.
- Ensure there is no pinching or pulling of the breast tissue around the flange.
- Use cushioned or soft silicone flanges if recommended or available.
Any severe or recurring bruising should be evaluated by a healthcare provider to rule out underlying issues.
7. Milk Contamination and Baby’s Gut Infections
Improper cleaning and storage of pump parts and breast milk can lead to milk contamination, which may cause infections in your baby.
Risk factors
- Not washing hands before handling pump or milk
- Leaving pump parts unwashed or wet for long periods
- Storing milk at unsafe temperatures
- Using unsterilised containers
Common symptoms in the baby
- Diarrhoea or loose stools
- Vomiting
- Fever
- Irritability, poor feeding
If your baby shows signs of infection, consult a pediatrician. They may order tests such as:
- Stool test for infection
- Blood tests to rule out serious infections
For mothers, monitoring overall immunity and health through routine health packages can also be useful, especially in the postpartum period.
8. Emotional Stress and Anxiety Related to Pumping
Pumping can sometimes feel stressful, especially when:
- You feel pressured to build a large milk stash
- You are balancing work and pumping schedules
- You are struggling with low output despite efforts
Impact on health
Chronic stress and sleep deprivation can affect milk supply, mental health, and overall recovery after childbirth.
What can help
- Set realistic expectations about pumping output.
- Take short breaks and practice relaxation techniques.
- Seek support from family, support groups, and lactation consultants.
- Discuss symptoms of anxiety or depression with your doctor.
Postpartum depression and anxiety are medical conditions and may require professional care and, sometimes, lab evaluation to rule out contributing factors like anemia or thyroid imbalance. Relevant tests from Seralis Lab include:
Long-Term Considerations of Frequent Breast Pump Use
Most side effects of pumping are temporary and improve with correct technique. However, long-term heavy reliance on pumping without guidance may contribute to:
- Chronic nipple or breast pain
- Recurrent mastitis
- Fluctuations in milk supply
- Burnout, stress, and sleep disruption
Regular follow-ups with your gynecologist or lactation consultant can help you maintain a healthy, sustainable pumping routine.
How to Use a Breast Pump Safely
1. Choose the Right Pump and Flange Size
- Follow manufacturer recommendations for nipple and areola measurements.
- Ensure the nipple moves freely in the flange tunnel without excessive areola being pulled in.
2. Maintain Strict Hygiene
- Wash hands before touching pump parts or breasts.
- Disassemble and clean all parts that touch milk after each use with warm soapy water, and allow to air-dry completely.
- Sterilise according to manufacturer guidelines (especially for newborns or preterm babies).
3. Use Appropriate Suction and Duration
- Begin with low suction and gradually increase until you find a comfortable, effective level.
- Typical session duration: 15–20 minutes per breast, or as advised by your healthcare provider.
4. Store Expressed Milk Safely
- Use sterile containers or milk storage bags.
- Follow recommended storage times (e.g., up to 4 hours at room temperature, up to 4 days in refrigerator, and longer in freezer — depending on guidelines your doctor follows).
- Label milk with date and time.
5. Listen to Your Body
- Stop pumping if you experience sharp pain.
- Monitor your breasts regularly for lumps, redness, or unusual changes.
- Seek medical help if symptoms do not improve within a day or two.
When to See a Doctor
Consult your doctor or lactation consultant if you notice:
- Persistent nipple pain, cracks, or bleeding
- Swelling, hard lumps, or warmth in the breast
- Fever, chills, and flu-like symptoms (possible mastitis)
- Sudden drop in milk supply despite proper pumping
- Signs of infection in your baby after feeding expressed milk
Your doctor may recommend lab tests through trusted diagnostic centers. You can book relevant investigations and postpartum health packages at Seralis Lab, including:
- Complete Blood Count (CBC) – to assess infection and anemia.
- CRP / ESR (Inflammatory Markers) – if your doctor suspects active infection or inflammation.
- Thyroid Profile – to evaluate hormonal causes of low milk supply or fatigue.
- Postnatal / Women’s Wellness Packages – comprehensive screening for new mothers.
Relevant Tests and Packages from Seralis Lab
To support your breastfeeding journey and overall postpartum health, consider these Seralis Lab offerings:
1. Postnatal Health Check Packages
These typically include:
- CBC (for anemia, infection)
- Thyroid Profile
- Blood Sugar and Lipid Profile
- Key vitamins and minerals, depending on package
View Postnatal Health Packages on Seralis Lab
2. Infection & Inflammation Tests
- Complete Blood Count (CBC)
- C-Reactive Protein (CRP)
- ESR (Erythrocyte Sedimentation Rate)
3. Hormonal & Nutritional Panels
- Thyroid Function Tests (T3, T4, TSH)
- Vitamin D and Vitamin B12 (for fatigue, low mood, and overall recovery)
- Iron Studies / Anemia Profile
Speak with your doctor about which tests are most relevant for your specific symptoms, then book them easily through Seralis Lab.
Key Takeaways
- Breast pumps are helpful tools but can cause nipple pain, breast trauma, infections, and emotional stress if not used correctly.
- Correct flange size, proper suction, and hygiene are essential to minimise side effects.
- Watch for warning signs like severe pain, lumps, redness, or fever, and seek medical care promptly.
- Postpartum health checks and targeted lab tests through Seralis Lab can help monitor your recovery and address complications early.
Always discuss your pumping routine and any symptoms with your gynecologist, pediatrician, or a certified lactation consultant to ensure a safe and comfortable breastfeeding journey.
FAQs on Breast Pump Side Effects
1. Is it safe to use a breast pump every day?
Yes, many mothers use breast pumps daily, especially when working or when the baby cannot latch. It is safe as long as you:
- Use the correct flange size and comfortable suction level.
- Clean and sterilise pump parts properly.
- Monitor your breasts for pain, redness, or lumps.
2. Can using a breast pump cause breast cancer?
No current evidence suggests that using a breast pump causes breast cancer. Pumping can, however, reveal existing breast lumps earlier because you are regularly handling and observing your breasts. Any new or suspicious lump should be evaluated by a doctor.
3. Why do my nipples hurt when I pump?
Nipple pain is often due to:
- Incorrect flange size
- Excessive suction
- Prolonged pumping sessions
Adjust these factors and seek help from a lactation consultant. If pain persists or nipples crack or bleed, consult your gynecologist.
4. How do I know if I have mastitis from pumping?
Symptoms of mastitis include:
- Red, painful area on the breast
- Fever, chills, and flu-like feelings
- Body aches and severe fatigue
If you suspect mastitis, seek medical care immediately. Your doctor may suggest antibiotics and, if needed, tests such as a CBC or inflammatory markers.
5. Can pumping reduce my milk supply?
Pumping itself does not reduce supply when done correctly. However, infrequent or incomplete pumping can signal your body to make less milk. Maintaining a regular schedule and emptying the breasts effectively helps sustain or increase supply.
6. How often should I replace my pump parts?
Follow the manufacturer’s recommendation, but in general:
- Valves and membranes may need replacement every few weeks to months, depending on use.
- Flanges and tubing should be replaced if cracked, discoloured, or not functioning properly.
7. Are there any tests I should do after delivery to support breastfeeding health?
Your doctor may recommend postpartum tests to ensure your recovery is on track. Common examples include:
- CBC (for anemia or infection)
- Thyroid profile
- Vitamin D, Vitamin B12, and iron levels
You can book these through Seralis Lab under their Postnatal Health Packages or individual test options.
References
- Academy of Breastfeeding Medicine. ABM Clinical Protocol #8: Human Milk Storage Information for Home Use for Full-Term Infants.
- World Health Organization (WHO). Breastfeeding – Key Facts.
- Centers for Disease Control and Prevention (CDC). Proper Storage and Preparation of Breast Milk.
- Amir LH. Breast pain in lactating women – Mastitis or something else? Australian Family Physician. 2003.
- Spatz DL. Preventing engorgement and mastitis in breastfeeding women. Journal of Perinatal & Neonatal Nursing. 2012.
- Centers for Disease Control and Prevention (CDC). Breast Pump Cleaning Guidelines.
- Victora CG, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet. 2016.